New rules ignite a surge in payer demand for data platforms that support RADV readiness, Stars forecasting, and member retention analytics.
WASHINGTON, DC / ACCESS Newswire / May 23, 2025 / In the wake of this week's Centers for Medicare & Medicaid Services (CMS) announcement mandating annual RADV audits for all Medicare Advantage (MA) plans, health insurers face unprecedented urgency to modernize their audit readiness, risk adjustment, and quality performance infrastructure.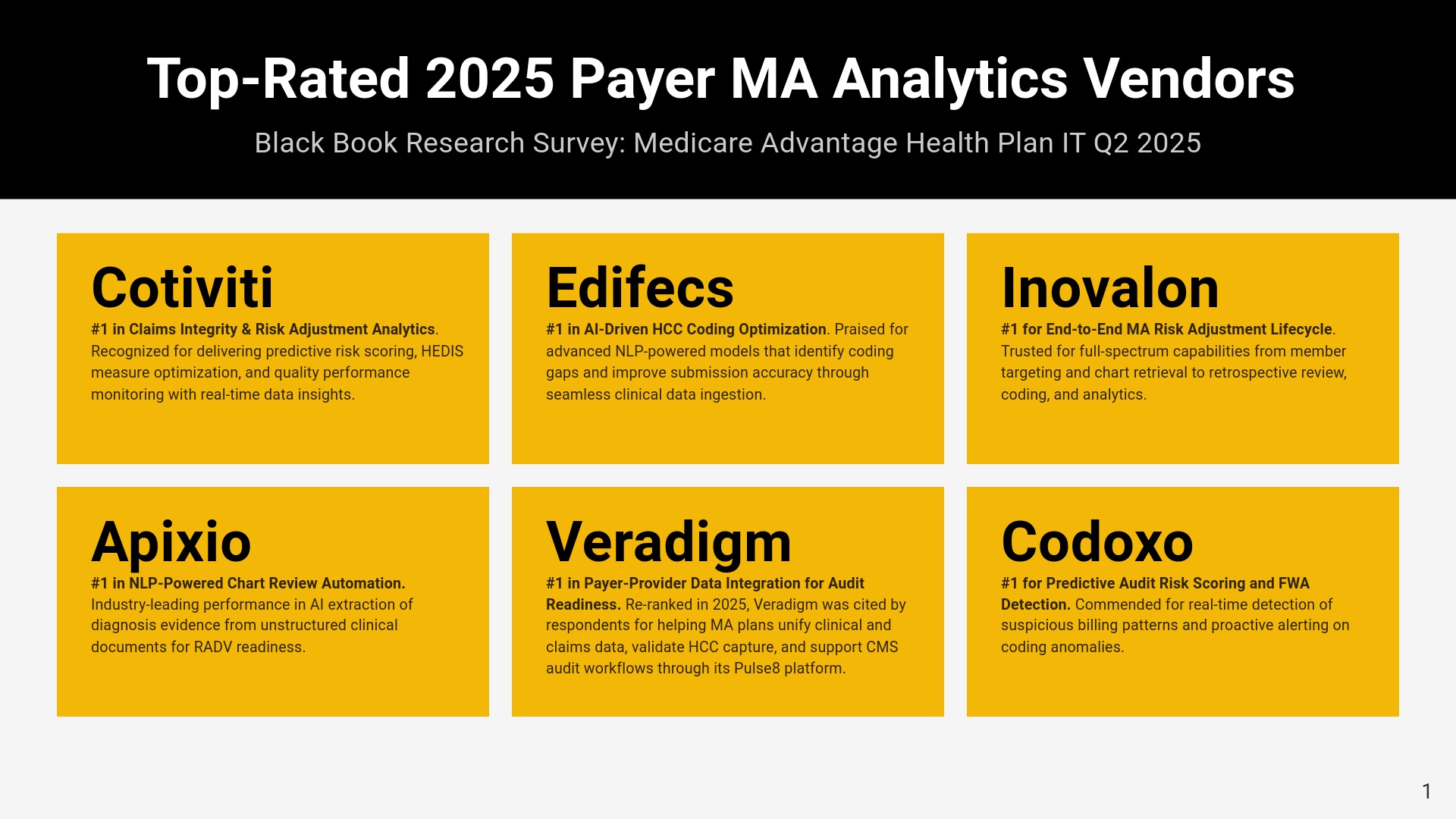
Today, Black Book Research reintroduces its 2025 top-rated payer analytics vendors, independently evaluated by 972 MA IT, finance, and operations leaders. These firms are recognized for enabling plans to navigate CMS's tightening regulatory scrutiny while also supporting superior Star Ratings, member outcomes, and audit compliance.
"CMS's aggressive audit expansion demands more than risk scoring and it requires a complete transformation of how MA plans use data," said Doug Brown, Founder of Black Book. "These top-rated vendors provide the analytics backbone for audit defensibility, quality improvement, and real-time operational control."
Top 2025 Medicare Advantage Analytics Vendors
Based on client satisfaction scores across 18 performance indicators including RADV readiness, coding accuracy, real-time insights, and population health impact these vendors earned top recognition in the Black Book Midyear MA Analytics Rankings:
Cotiviti - #1 in Claims Integrity & Risk Adjustment Analytics
Cotiviti earned top honors for its unmatched ability to detect payment inaccuracies, close risk adjustment gaps, and drive compliance with CMS audit standards through integrated claims analytics and retrospective data validation.
Edifecs - #1 in AI-Driven HCC Coding Optimization
Edifecs was ranked #1 for its AI-powered risk adjustment suite that automates HCC suspect identification, reduces coding variance, and aligns seamlessly with Medicare Advantage compliance requirements.
Inovalon - #1 for End-to-End MA Risk Adjustment Lifecycle
Inovalon was recognized for its comprehensive risk adjustment ecosystem, spanning encounter data aggregation, clinical documentation improvement, and Stars measure optimization within a unified platform.
Apixio - #1 in NLP-Powered Chart Review Automation
Apixio received the top ranking for pioneering the use of natural language processing to extract accurate diagnoses from unstructured medical records, significantly accelerating RADV audit readiness.
Veradigm - #1 in Payer-Provider Data Integration for Audit Readiness
Veradigm led this category for delivering real-time payer-provider interoperability tools that validate diagnosis accuracy, streamline data submission, and support proactive audit risk mitigation.
Health Fidelity (Edifecs) - #1 in Retrospective Risk Identification
Health Fidelity earned top placement by leveraging AI to surface unsupported or under-documented risk conditions through retrospective chart analysis, improving HCC capture and audit defensibility.
Codoxo - #1 for Predictive Audit Risk Scoring & FWA Detection
Codoxo was named #1 for its forensic AI engine that predicts audit vulnerabilities, flags anomalous provider patterns, and proactively prevents fraud, waste, and abuse across claims workflows.
SCIO Health Analytics (EXL) - #1 in Claims Outlier & Utilization Analytics
SCIO, a division of EXL, topped this category with its ability to uncover utilization anomalies and cost drivers through provider benchmarking, patient cohort analysis, and real-time outlier detection.
Each of these platforms demonstrated measurable impact on MA plan performance across quality metrics, documentation compliance, Stars forecasting, and HCC optimization. "The CMS audit expansion has made it clear that outdated analytics and fragmented data pipelines will no longer suffice," said Brown. "This year's top-rated MA plan analytics vendors didn't just provide tools, they delivered measurable outcomes tied directly to audit defense, risk scoring precision, and CMS quality benchmarks."
Expanding Analytics Beyond Risk Adjustment: 5 Emerging Categories in 2025
Drawing from the full 2025 Black Book report: Technology Enablers for High-Performing MA Plans, survey managers identified five additional high-priority analytics categories that are transforming how top-rated Medicare Advantage organizations manage CMS performance expectations. The top rated vendors will be announced on May 27.
Star Ratings Forecasting & Quality Improvement Analytics
Used to simulate the financial and operational impact of performance on CMS Star Ratings and prioritize interventions.
Real-Time Clinical Event Detection & Interventions
Platforms analyzing admission, discharge, and ED visit data for immediate outreach and case management.
Social Determinants of Health (SDoH) Analytics
Used to identify non-clinical risk factors and activate community interventions for quality compliance and equity.
Grievance, Appeals & Complaint Resolution Analytics
Vital for lowering disenrollment rates and meeting CMS audit timelines (ODAG/CDAG compliance).
Churn Risk and Member Retention Predictive Models
AI tools that score member loyalty risk, enabling personalized outreach to reduce attrition and boost NPS.
"These capabilities, combined with core audit and risk adjustment tools, have become defining traits of the 7 MA plans awarded 5-star ratings in 2025 including Highmark Health, Leon Health, and Optimum Healthcare. Each of these plans implemented multi-layered analytics ecosystems supporting CMS-aligned care coordination, documentation accuracy, member satisfaction, and compliance resilience." added Brown.
These vendors represent the top tier of analytics and compliance readiness tools in a market where average MA Star Ratings declined from 4.07 to 3.92, and only seven plans earned 5 stars, according to CMS.
For the full report, methodology, and vendor evaluation tables based on 18 qualitative KPIs, visit www.blackbookmarketresearch.com. The full report, released to media can be downloaded for no cost to industry stakeholders starting May 26 at https://blackbookmarketresearch.com/technology-enablers-for-high-performing-medicare-health-plans-2025
About Black Book™
Since 2004, Black Book™ has polled payers, providers, and health systems on IT and managed services vendors through a vendor-agnostic, independently financed methodology. Black Book's Medicare Advantage analytics rankings are derived from over 200,000 validated responses across 18 KPIs related to ROI, audit readiness, outcomes, and user experience. Since 2004, Black Book™ has polled payers, providers, and health systems on IT and managed services vendors through a vendor-agnostic, independently financed methodology. Black Book's Medicare Advantage analytics rankings are derived from over 200,000 validated responses across 18 KPIs related to ROI, audit readiness, outcomes, and user experience.
Black Book accepts no vendor influence, subscriptions, consulting fees, or performance improvement program sponsorships in its payer IT research process-ensuring results are entirely based on client experience and satisfaction.
Contact Information
Press Office
research@blackbookmarketresearch.com
8008637590
SOURCE: Black Book Research
View the original press release on ACCESS Newswire
